Alzheimer's disease: Difference between revisions
m (→Cause/etiology: one punctuation edit) |
(→Medications: a few changes to section including clarifying the effectiveness of one drug) |
||
| Line 147: | Line 147: | ||
As of 2023, available medications offer relatively small symptomatic benefit for some patients but generally do not slow disease progression. Newer monoclonal antibody treatments against beta-amyloid protein have been approved in the United States, but they only slightly reduce the rate of disease progression and have significant side effects, including brain bleeding and in rare cases, death. These drugs cost over $20,000 a year, which could be prohibitively expensive for many patients or insurance companies. | As of 2023, available medications offer relatively small symptomatic benefit for some patients but generally do not slow disease progression. Newer monoclonal antibody treatments against beta-amyloid protein have been approved in the United States, but they only slightly reduce the rate of disease progression and have significant side effects, including brain bleeding and in rare cases, death. These drugs cost over $20,000 a year, which could be prohibitively expensive for many patients or insurance companies. | ||
[[Randomized controlled trial]]s showed either small or absent benefit from | [[Randomized controlled trial]]s showed either small or absent benefit from acetylcholinesterase inhibitors<ref> | ||
{{cite journal | author = Kaduszkiewicz H, Zimmermann T, Beck-Bornholdt H, van den Bussche H | title = Cholinesterase inhibitors for patients with Alzheimer's disease: systematic review of randomised clinical trials. | journal = BMJ | {{cite journal | author = Kaduszkiewicz H, Zimmermann T, Beck-Bornholdt H, van den Bussche H | title = Cholinesterase inhibitors for patients with Alzheimer's disease: systematic review of randomised clinical trials. | journal = BMJ | ||
| volume = 331 | issue = 7512 | pages = 321-7 | year = 2005 | id = PMID 16081444}} </ref> such as donepezil.<ref name="pmid17914039"> {{cite journal |author=Howard RJ, Juszczak E, Ballard CG, ''et al'' |title=Donepezil for the treatment of agitation in Alzheimer's disease |journal=N. Engl. J. Med. |volume=357 |issue=14 |pages=1382–92 |year=2007 |pmid=17914039 | | volume = 331 | issue = 7512 | pages = 321-7 | year = 2005 | id = PMID 16081444}} </ref> such as donepezil.<ref name="pmid17914039"> {{cite journal |author=Howard RJ, Juszczak E, Ballard CG, ''et al'' |title=Donepezil for the treatment of agitation in Alzheimer's disease |journal=N. Engl. J. Med. |volume=357 |issue=14 |pages=1382–92 |year=2007 |pmid=17914039 | ||
| Line 153: | Line 153: | ||
| issue = 9427 | pages = 2105-15 | year = 2004 | id = PMID 15220031}}</ref><ref name="doi10.1056/NEJMoa1106668">Donepezil and Memantine for Moderate-to-Severe Alzheimer's Disease. NEJM 2012. http://dx.doi.org/10.1056/NEJMoa1106668</ref> | | issue = 9427 | pages = 2105-15 | year = 2004 | id = PMID 15220031}}</ref><ref name="doi10.1056/NEJMoa1106668">Donepezil and Memantine for Moderate-to-Severe Alzheimer's Disease. NEJM 2012. http://dx.doi.org/10.1056/NEJMoa1106668</ref> | ||
The [[N-methyl-d-aspartate receptor]] antagonist | The [[N-methyl-d-aspartate receptor]] antagonist memantine has shown some effectiveness<ref name="Areosa"> | ||
{{cite journal | author = Areosa Sastre A, McShane R, Sherriff F | title = Memantine for dementia. | {{cite journal | author = Areosa Sastre A, McShane R, Sherriff F | title = Memantine for dementia. | ||
| journal = Cochrane Database Syst Rev | pages = CD003154 | id = PMID 15495043}}</ref> but does not add benefit to donepezil .<ref name="doi10.1056/NEJMoa1106668"/> | | journal = Cochrane Database Syst Rev | pages = CD003154 | id = PMID 15495043}}</ref> but does not add benefit to donepezil .<ref name="doi10.1056/NEJMoa1106668"/> | ||
Revision as of 10:09, 30 December 2023
| Alzheimer's disease | |
|---|---|
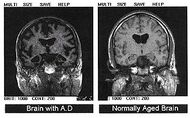
| Post-autopsy brain scans: A brain with Alzheimer's disease (left) as compared to a normal brain (right) | |
| ICD-10 | ICD10 F84.0-F84.1, ICD10 F84.0-F84.1 |
| ICD-9 | 331.0 |
| OMIM | 104300 |
| MedlinePlus | 000760 |
Alzheimer's disease is also known as Alzheimer disease, Alzheimer's and simply AD.
Alzheimer's is the most common cause of dementia, afflicting at least 24 million people worldwide. Alzheimer's is a terminal disease for which there is currently no known cure. It is most commonly found in people over 65 years old, although a less-common form called Familial Alzheimer's disease, or "early-onset Alzheimer's", also occurs, affecting about 1%—5% of the total of Alzheimer's sufferers.[1]
Typically, the disease begins many years before it is diagnosed. In its early stages, short-term memory loss is the most common symptom, which is often initially thought by the sufferer to be caused by other factors, such as aging or stress.[2] Later symptoms of the disease include confusion, anger, mood swings, language breakdown, long-term memory loss, and the general "withdrawal" of the sufferer as his or her senses decline.[2][3] Gradually the sufferer will lose minor, and then major bodily functions, until death finally occurs.[4] Survival after diagnosis has been estimated to be between 5 and 20 years.[5][6]
Classification
A classification has been proposed by the the ad hoc International Working Group for New Research Criteria for the Diagnosis of AD.[7]
Asymptomatic at-risk for Alzheimer's disease
Asymptomatic at-risk for Alzheimer's disease includes asymptomatic patients with a positive biomarker. Biomarkers include apolipoprotein E4.
Presymptomatic Alzheimer's disease
Presymptomatic Alzheimer's disease includes people with autosomal dominant mutation known to have full penetrance
Prodromal Alzheimer's disease
Prodromal Alzheimer's disease includes patients with positive biomarkers who have mild cognitive dysfunction that does not cause significant functional impairment.
Alzheimer's Dementia
Alzheimer's dementia indicates functional impairment meeting criteria for dementia.
Symptoms
Common symptoms of dementia include:
A decline in memory Changes in thinking skills Poor judgment and reasoning Decreased focus and attention Decreased language ability Negative changes in behavior
Although the symptoms are common, they are typically experienced in unique ways.[8] "Stages" are commonly referred to by professionals to describe the progressive nature of Alzheimer's (typically "early", "mid" and "late onset") but the symptoms can cross over these "boundaries" for many sufferers.
Diagnosis
The symptoms of Alzheimer's disease are generally reported to a doctor or physician when memory-loss (or symptoms surrounding memory loss) begin to pose a serious concern. When Alzheimer's disease is suspected, diagnosis is typically confirmed by a behavioural assessment, and some form of cognitive test. Often this is followed by a brain scan.[9]
Laboratory tests
Apolipoprotein E4
Although apolipoprotein E4 is an important susceptibility gene for Alzheimer's disease][10], its sensitivity and specificity are insufficient (65 and 68 percent, respectively) to be used as a diagnostic test.[11]
However, the level of apolipoprotein E4 in cerebrospinal fluid may be predictive.[12]
Amyloid-beta protein
Amyloid-beta protein may be elevated in the cerebrospinal fluid of some patients.[12]
Cause/etiology
The etiology of Alzheimer's disease is incompletely understood. Alzheimer's disease is associated with senile plaques and neurofibrillary tangles in the brain.[13] The incorrect folding of proteins leads to the formation of amyloid plaques. The prion protein (PrPC) may be the cellular receptor for amyloid-beta oligomer.[14] Current research aims to determine if such plaques are the result of, or the cause of, Alzheimer's disease.
Regarding biomarkers, one study found that "a reduction in the CSF Aβ42 level denotes a pathophysiological process that significantly departs from normality (ie, becomes dynamic) early, whereas the CSF total tau level and the adjusted hippocampal volume are biomarkers of downstream pathophysiological processes". [15]
Although there is a genetic susceptibility in a small percentage of people, Alzheimer's is not considered a genetic illness. Major risk factors include a diet high in saturated fats that are typical of the standard western diet, smoking, and long-term exposure to environmental toxins such as aluminum. Research is ongoing.
Treatment
No treatment has been found to stop or reverse the disease. Many preventive measures have been suggested for Alzheimer's disease, but their values are uncertain: mental stimulation, exercise, and a Mediterranean style diet are usually recommended, both as possible prevention and as a sensible way of managing the disease.[16]
Medications
As of 2023, available medications offer relatively small symptomatic benefit for some patients but generally do not slow disease progression. Newer monoclonal antibody treatments against beta-amyloid protein have been approved in the United States, but they only slightly reduce the rate of disease progression and have significant side effects, including brain bleeding and in rare cases, death. These drugs cost over $20,000 a year, which could be prohibitively expensive for many patients or insurance companies.
Randomized controlled trials showed either small or absent benefit from acetylcholinesterase inhibitors[17] such as donepezil.[18][19][20]
The N-methyl-d-aspartate receptor antagonist memantine has shown some effectiveness[21] but does not add benefit to donepezil .[20]
Care management
Due to the incurable and degenerative nature of the disease care-management of Alzheimer's is essential. The role of the main caregiver is often taken by the spouse or a close relative.[22] Caregivers may themselves suffer from stress, over-work, depression, and from being physically assailed.[23]
Alzheimer's in society
Famous people who have, or have died of Alzheimer's disease, are the US president Ronald Reagan, the UK Prime minister Harold Wilson, the writers Terry Pratchett and Iris Murdoch, and the film stars Rita Hayworth and Charlton Heston.
History
Alzheimer’s disease is named after Dr. Alois Alzheimer, the German physician who first described it. In 1901, Alzheimer observed a 51-year-old patient at the Frankfurt asylum named Auguste Deter. Her symptoms included memory loss, language problems, and unpredictable behavior. In 1906, she died and Dr. Alzheimer noticed unusual pathology in her brain tissue; he found many abnormal clumps (now called amyloid plaques) and tangled bundles of fibers (now called neurofibrillary, or tau, tangles).
References
- ↑ Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, Hasegawa K, Hendrie H, Huang Y, Jorm A, Mathers C, Menezes PR, Rimmer E, Scazufca M (2005). "Global prevalence of dementia: a Delphi consensus study". Lancet 366 (9503): 2112–2117. DOI:10.1016/S0140-6736(05)67889-0. PMID 16360788. Research Blogging.
- ↑ 2.0 2.1 Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rossor M, Scheltens P, Tariska P, Winblad B (2007). "Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline". European Journal of Neurology 14 (1): E1–26. DOI:10.1111/j.1468-1331.2006.01605.x. PMID 17222085. Research Blogging.
- ↑ Tabert MH, Liu X, Doty RL, Serby M, Zamora D, Pelton GH, Marder K, Albers MW, Stern Y, Devanand DP (2005). "A 10-item smell identification scale related to risk for Alzheimer's disease". Ann. Neurol. 58 (1): 155–60. DOI:10.1002/ana.20533. PMID 15984022. Research Blogging.
- ↑ Understanding Stages and Symptoms of Alzheimer's Disease. National Institute on Aging (2007-10-26). Retrieved on 2008-02-21.
- ↑ Alzheimer's Disease Information Page. National Institute of Neurological Disorders and Stroke (NINDS) (2008-02-07). Retrieved on 2008-02-12.
- ↑ Alzheimer's Disease Treatment and Prognosis. Healthlink. Retrieved on 2008-02-15.
- ↑ Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P et al. (2010). "Revising the definition of Alzheimer's disease: a new lexicon.". Lancet Neurol 9 (11): 1118-27. DOI:10.1016/S1474-4422(10)70223-4. PMID 20934914. Research Blogging.
- ↑ What is Alzheimer’s disease?. www.alzheimers.org.uk (August 2007). Retrieved on 2008-02-21.
- ↑ Alzheimer's Diagnosis of AD. Alzheimer's Reearch Trust. Retrieved on 2008-02-29.
- ↑ Skoog I (August 2000). "Detection of preclinical Alzheimer's disease". N. Engl. J. Med. 343 (7): 502–3. PMID 10944568. “The APOE 4 allele is a susceptibility gene for Alzheimer's disease and seems to affect the age of onset of the disease. However, the presence of this allele alone is not sufficient to predict which asymptomatic subjects will ultimately have Alzheimer's disease, and the disease never develops in many subjects with this genotype” [e]
- ↑ Kivipelto M, Helkala EL, Laakso MP, et al (August 2002). "Apolipoprotein E epsilon4 allele, elevated midlife total cholesterol level, and high midlife systolic blood pressure are independent risk factors for late-life Alzheimer disease". Ann. Intern. Med. 137 (3): 149–55. PMID 12160362. [e]
- ↑ 12.0 12.1 De Meyer G, Shapiro F, Vanderstichele H, Vanmechelen E, Engelborghs S, De Deyn PP et al. (2010). "Diagnosis-independent Alzheimer disease biomarker signature in cognitively normal elderly people.". Arch Neurol 67 (8): 949-56. DOI:10.1001/archneurol.2010.179. PMID 20697045. Research Blogging.
Cite error: Invalid
<ref>tag; name "pmid20697045" defined multiple times with different content - ↑ Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J (2004). "The importance of neuritic plaques and tangles to the development and evolution of AD". Neurology 62 (11): 1984–1989. PMID 15184601. [e]
- ↑ Laurén J, Gimbel DA, Nygaard HB, Gilbert JW, Strittmatter SM (February 2009). "Cellular prion protein mediates impairment of synaptic plasticity by amyloid-beta oligomers". Nature 457 (7233): 1128–32. DOI:10.1038/nature07761. PMID 19242475. Research Blogging.
- ↑ Jack CR, Vemuri P, Wiste HJ, Weigand SD, Aisen PS, Trojanowski JQ et al. (2011). "Evidence for ordering of Alzheimer disease biomarkers.". Arch Neurol 68 (12): 1526-35. DOI:10.1001/archneurol.2011.183. PMID 21825215. Research Blogging.
- ↑ The Search for AD Prevention Strategies. National Institute on Aging (2006-08-29). Retrieved on 2008-02-29.
- ↑ Kaduszkiewicz H, Zimmermann T, Beck-Bornholdt H, van den Bussche H (2005). "Cholinesterase inhibitors for patients with Alzheimer's disease: systematic review of randomised clinical trials.". BMJ 331 (7512): 321-7. PMID 16081444.
- ↑ Howard RJ, Juszczak E, Ballard CG, et al (2007). "Donepezil for the treatment of agitation in Alzheimer's disease". N. Engl. J. Med. 357 (14): 1382–92. DOI:10.1056/NEJMoa066583. PMID 17914039. Research Blogging.
- ↑ Courtney C, Farrell D, Gray R, Hills R, Lynch L, Sellwood E, Edwards S, Hardyman W, Raftery J, Crome P, Lendon C, Shaw H, Bentham P (2004). "Long-term donepezil treatment in 565 patients with Alzheimer's disease (AD2000): randomised double-blind trial.". Lancet 363 (9427): 2105-15. PMID 15220031.
- ↑ 20.0 20.1 Donepezil and Memantine for Moderate-to-Severe Alzheimer's Disease. NEJM 2012. http://dx.doi.org/10.1056/NEJMoa1106668
- ↑ Areosa Sastre A, McShane R, Sherriff F. "Memantine for dementia.". Cochrane Database Syst Rev: CD003154. PMID 15495043.
- ↑ O’Donovan ST. "Dementia caregiving burden and breakdown" (PDF). Retrieved on 2008-02-29.
- ↑ Selwood A, Johnston K, Katona C, Lyketsos C, Livingston G (2007). "Systematic review of the effect of psychological interventions on family caregivers of people with dementia". Journal of Affective Disorders 101 (1-3): 75–89. DOI:10.1016/j.jad.2006.10.025. PMID 17173977. Research Blogging.